Thousands of revenue dollars, if not hundreds of thousands, are lost every year due to missed charges. One significant reason is that many practices lack an adequate reconciliation process to ensure every exam is properly coded and billed. Relying solely on matching the accession number to what was ordered and what was billed is not sufficient. Many organizations don’t know which or how many charges are missed, let alone what they amount to. Others that do have visibility may not be able to rapidly take remediation steps before a claims submission deadline. The result is lost revenue that leads to diminished financial health: less staff to meet growing demand, less capital investments, and limited growth.
Recovering Revenue
Summit Radiology Services (Summit), a Georgia practice that supports over 14 hospitals, is bridging the gap between missed charges and accurate billing. Every day, they conduct an audit procedure that identifies missed charges to recover thousands of dollars that would have otherwise been lost. They also identify underbilled charges, e.g., a retroperitoneal ultrasound coded as limited versus complete when documentation provides the left/right kidney & bladder along with a urinary tract indication. Core to their process is Foundations™; its powerful auditing and verbiage search capabilities give Summit unmatched, timely visibility into their records to identify gaps and recover revenue.
“Because of Foundations™, we’re able to identify over 97% of missed charges,” says Summit’s Director of RCM (Coding & Compliance), Christy Hembree. “Rapidly identifying billing discrepancies streamlines our auditing process across high volumes, ensuring timely corrections that maintain compliance with payor guidelines.”
Intuitive Audits
Using Foundations™, Summit follows an intuitive process that gives them a detailed, step-by-step look into their billings. First, they review a table populated with rows of phrases commonly associated with procedures. Examples include “3D”, “ANGIOGRAM HEAD,” and “CT COMBO CHEST ABDOMEN PELVIS.” Summit can modify these results when they add or exclude phrases and codes.
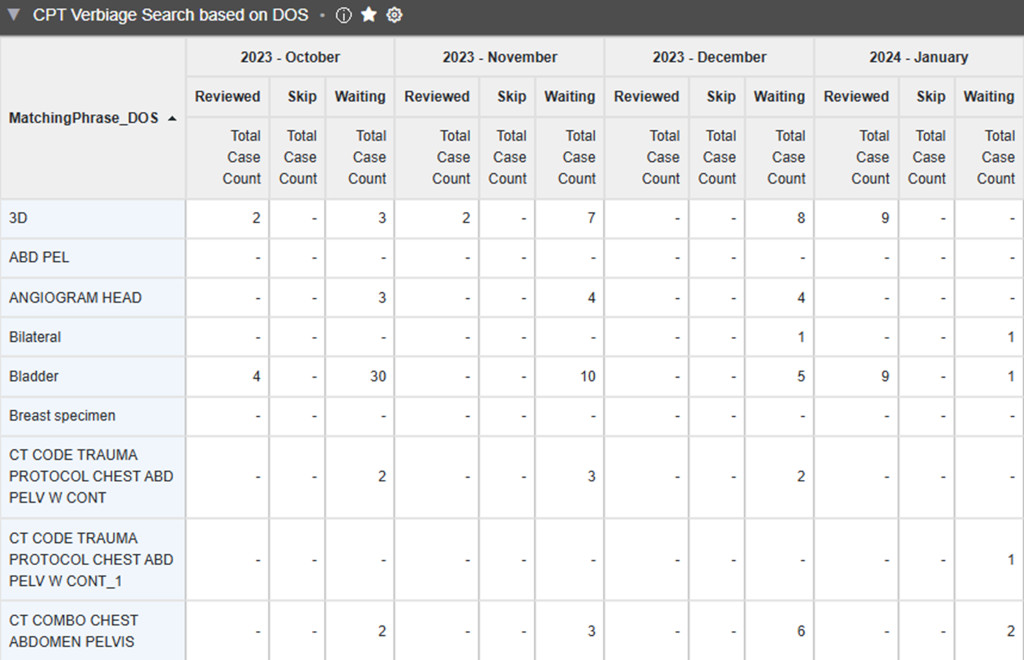
Columns list the number of monthly cases with missed charges discovered by Foundations™. They are placed into Reviewed, Skipped, and Waiting to be Reviewed statuses. Clicking on a case in Waiting to be Reviewed, for example, brings up the associated case report. After Summit confirms that the Foundations™-identified codes are missing in the billing system, they notify their billing partner of the new charges (using Foundations™).
“When the reconciliation process solely relies on accession numbers, a practice may overlook specific add-on or combo procedures,” says Christy. “Commonly missed charges include CTA or MRA head/neck combos, sedation, and bilateral exams. This leads to missed charges that could impact a practice’s bottom line. With Foundations™, it’s not just about accession numbers, but about verifying each unique charge to improve revenue integrity.”
Revenue Integrity Matters
Practices and imaging centers are facing increasing strain due to the rising demand for services. Those with adequate gross revenue are better positioned to scale up their operational needs to meet these demands, including growing staff and infrastructure. Others, like Summit Radiology Services, are boosting their revenue integrity by recovering dollars from missed or underbilled charges. With an intuitive, indispensable solution like Foundations™, radiology businesses can strengthen their financial health and remain competitive within the increasingly competitive radiology landscape.


Recent Comments